“Patients and doctors often find it difficult to speak openly about preparing for death”
Workshop on Advance Care Planning
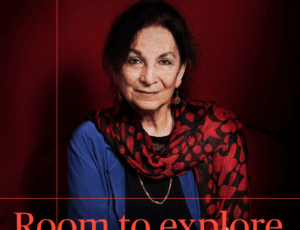
18 June 2014When a patient hears that ‘nothing more can be done’ and that they will probably die soon, clear timely communication between patient, their family, carers and health professionals is of the essence. However, according to healthcare scientist Judith Rietjens, this is not always the case. This week, an international workshop organised by Judith Rietjens will be held at NIAS to discuss the issue of communication in the context of caring for patients during the period around the end of life.
A charged topic
“Communication at the end of life is very complex,” says Rietjens, assistant professor at Erasmus Medical Center, Rotterdam. “Doctors sometimes find it problematic to speak openly with their patients about end of life especially if, for example, they cannot provide any certainty about how long the patient still has to live. Patients and their loved ones are often not able to express what they feel as they are distressed or afraid it might appear as though they have given up hope.” The consequence is that doctors are not always aware of their patients’ wishes, which sometimes results in patients being given care they didn’t really want, such as being admitted to hospital for the last few days before they die.
Discussing patient choices
In the US, a programme called ‘Respecting Choices’ has been developed to make sure each patient’s wishes are discussed in the right way and at the right time. This method of advanced care planning involves a structured form of communication in which the wishes and values of patients, and their next of kin, are discussed under the guidance of a trained counsellor – usually a nurse. Rietjens, “Patients are encouraged to discuss health choices with their doctors as an ongoing process in addition to writing a living will. If circumstances change, they can review their choices. A trained counsellor encourages the patient to share their feelings and wishes with family and friends.”
Advanced care planning is already commonly used in the US, Australia and Singapore but the effects on patients’ quality of life have barely been researched. This is what Judith Rietjens and her colleagues will attempt to do over the coming years as part of a European project that studies over 1300 patients with lung cancer or metastic colon cancer, from twenty hospitals in six different European countries. During the workshop at NIAS, with experts such as professors Bud Hammes and Rebecca Sudore from the US, the current state of advanced care planning will be mapped out and plans drawn up for the future.
“Advanced care planning has the potential to ensure that medical care is delivered more in line with patients’ wishes. Whether this is actually happens remains to be seen,” says Rietjens, “but we hope that the quality of life for patients in their final stages will be improved by this programme”.
For Women in Science
The invitational workshop “Advanced Care Planning: Interdisciplinary Perspectives” (19 and 20 June 2014) will be held at NIAS and is part of the Dutch L’Oréal-UNESCO For Women in Science Fellowship awarded to Judith Rietjens in 2012. This fellowship was initiated by L’Oréal, UNESCO, the Dutch Network of Women Professors and NIAS to stimulate the careers of talented young female researchers and to contribute to redressing the balance of women professors in the Netherlands.